
Mitral Valve Prolapse (MVP)
- Mitral Valve Prolapse (MVP)
- What are the Causes of Mitral Valve Prolapse?
- What is the Incidence Rate of Mitral Valve Prolapse?
- Is Mitral Valve Prolapse a Genetic Disease?
- What are the Diagnostic Methods for Mitral Valve Prolapse?
- What are the Symptoms of Mitral Valve Prolapse?
- What are the Treatment Methods for MVP?
In today's healthcare services and increased accessibility, early diagnosis and awareness have improved for many diseases, including heart valve disorders. MVP frequently emerges as a problem that is either not understood or overlooked by patients or, in some cases, overly emphasized, causing challenges for both the physician and the patient.
What are the Causes of Mitral Valve Prolapse?
MVP is a condition that occurs due to changes in components like collagen in the structure of the mitral valve. These changes result in thickening, heaviness, and altered elasticity of the valve, leading to insufficient functioning of the leaflets that are pushed toward the left atrium by blood with each heartbeat. Depending on the alterations the valve undergoes, significant tension can develop on the supporting cords, potentially causing ruptures and worsening valve leakage.
What is the Incidence Rate of Mitral Valve Prolapse?
MVP is a common valve disorder encountered in the community, with an incidence rate of 1.2% to 3%. It was first described in 1886 by Cuffer and Barbillon through auscultation findings, and later in 1936 by Barlow through physical examination findings. Due to its clinical heterogeneity, MVP still presents challenges in terms of diagnosis, treatment, and etiological investigations.
Is Mitral Valve Prolapse a Genetic Disease?
Yes, MVP is a genetically inheritable condition. Approximately 35-50% of first-degree relatives of MVP patients may have MVP as well. This can be attributed to a mutation on the X chromosome. Other gene mutations have also been identified in animal studies. Additionally, MVP can develop secondary to certain collagen disorders, connective tissue diseases, and bone diseases. The mitral valve annulus, a saddle-shaped structure, extends toward the left ventricle of the heart with its anterior and posterior parts at the apex. Mitral valve prolapse refers to the anterior and posterior parts exceeding the highest points of their levels during the movement of blood caused by cardiac contraction.
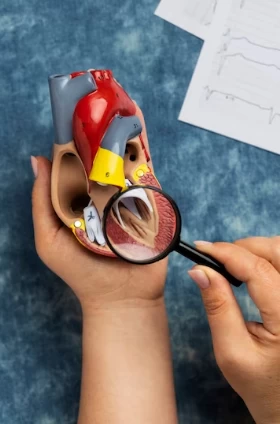
What are the Diagnostic Methods for Mitral Valve Prolapse?
The easiest and quickest diagnostic method in clinical practice is echocardiography performed alongside physical examination. However, a more comprehensive and reliable diagnostic test is cardiac magnetic resonance imaging.
What are the Symptoms of Mitral Valve Prolapse?
Patients commonly present with complaints of chest pain, exertional dyspnea, and palpitations. The most typical finding during physical examination is the presence of a mid-systolic click, an extra sound heard between two heartbeats. Although most patients do not experience significant events throughout their lives, patients between the ages of 40 and 60 can present with severe cardiac events. The risk of developing a serious complication throughout a lifetime is close to one-third of patients. MVP is the most common cause of isolated mitral regurgitation requiring surgical repair. Around 10% of familial cases experience sudden cardiac death. The risk of death is three times higher compared to the general population. Some patients may develop significant rhythm disturbances. Certain features determine whether patients are at higher risk, and this can be predicted based on ECG, echocardiography, and MRI findings.
What are the Treatment Methods for MVP?
Surgery is generally the successful treatment method. Although hypertension medications are used to reduce the workload on the valve, they do not prevent disease progression. The goal of surgery is to reduce the tension on the supporting muscle fibers and reshape the heart chambers to prevent deformation. This will reduce the occurrence of rhythm disturbances. Surgical methods include valve repair and replacement.
Beta-blockers are preferred for suppressing or treating rhythm disturbances. Treatment can be administered for significant rhythm disturbances, regardless of symptoms. Sometimes, electrophysiological studies are required to completely eliminate rhythm disturbances.
Advancements in genetic and molecular techniques may explain the genetic cause of MVP and enable preventive treatments to prevent the development of complications. Studies conducted on mice have demonstrated a mutation causing MVP, and changes in the valve were prevented through neutralizing antibodies. This indicates that disease progression can be prevented through future medical treatments.
In conclusion, the risks associated with this valve problem decrease when it is monitored. Therefore, patients should be regularly followed up and monitored when symptoms worsen. Additionally, screening of first-degree relatives of patients is advisable.




