Diabetic Retinopathy
- Diabetic Retinopathy
- What Is Diabetes?
- What Is Diabetic Retinopathy?
- What Are the Causes of Diabetic Retinopathy?
- What Are the Symptoms of Diabetic Retinopathy?
- How Is Diabetic Retinopathy Diagnosed?
- What Are the Treatment Options for Diabetic Retinopathy?
Diabetic retinopathy is an eye condition that arises as a complication of diabetes, a metabolic disorder commonly known as "sugar disease." Diabetic retinopathy affects the inner layer of the eye called the retina. Prolonged uncontrolled diabetes increases the risk of developing this condition, which can become a serious problem leading to blindness. In this article, I will provide more information about diabetic retinopathy, including its causes, symptoms, diagnosis methods, and treatment options.
What Is Diabetes?
First, let's recall what diabetes is. Diabetes, commonly known as sugar disease, is a metabolic disorder where the body's ability to regulate blood sugar (glucose) is impaired. The human body uses glucose as an energy source. Glucose is used by body cells to produce energy and circulates in the bloodstream. Insulin, a hormone, regulates the entry of glucose into cells and keeps blood sugar at normal levels.
Diabetes occurs when insulin is either not produced effectively or is not produced in sufficient quantities. As a result, maintaining normal blood sugar levels becomes challenging, leading to elevated blood sugar levels. There are two main types of diabetes:
- Type 1 Diabetes: Type 1 diabetes usually appears in childhood or youth. This type is characterized by the loss of the pancreas's ability to produce insulin due to an autoimmune reaction. Type 1 diabetes patients must use insulin injections or an insulin pump throughout their lives. They cannot survive without insulin.
- Type 2 Diabetes: Type 2 diabetes typically occurs in adults, especially in middle age and beyond. In this type, body cells become resistant to insulin, and the pancreas gradually fails to produce enough insulin. Most cases of type 2 diabetes are associated with lifestyle factors, obesity, physical inactivity, and genetic predisposition. Initially, attempts are made to control blood sugar through diet, exercise, and medications. In advanced cases, insulin therapy may be required.
What Is Diabetic Retinopathy?
Diabetic retinopathy is a disease that affects the eyes of diabetes patients, specifically targeting the inner layer of the eye called the retina. Diabetes, a condition that results from insufficient production or utilization of insulin, causes high blood sugar levels, which, when uncontrolled for an extended period, can lead to the development of diabetic retinopathy. The disease damages the blood vessels in the retina, leading to vision loss.

What Are the Causes of Diabetic Retinopathy?
The primary cause of diabetic retinopathy is the prolonged inability to control high blood sugar levels, which damages blood vessels. This condition leads to swelling, narrowing, or blockage of blood vessels within the eye. Other factors that can trigger diabetic retinopathy include:
- Duration of diabetes: The longer a person has diabetes, the higher the risk of developing diabetic retinopathy.
- Blood pressure control: High blood pressure can cause more significant damage to the retina.
- Genetic factors: Family history can influence the risk of diabetic retinopathy.
- Type of diabetes: Type 1 diabetes patients are at risk of diabetic retinopathy compared to type 2 diabetes patients.
What Are the Symptoms of Diabetic Retinopathy?
In the early stages of diabetic retinopathy, symptoms are often not noticeable. However, as the disease progresses, the following symptoms may emerge:
- Blurry vision
- Spots, dots, or gaps in the field of vision
- Difficulty seeing at night
- Altered or faded colors
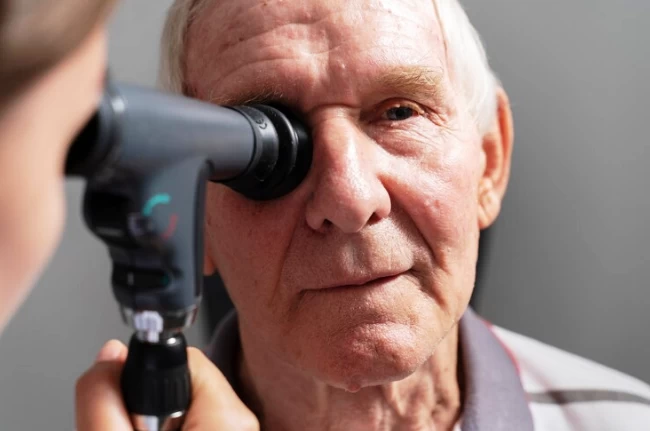
- Eye examination: We examine your eyes using a special lamp and lens to inspect the retina.
How Is Diabetic Retinopathy Diagnosed?
The diagnosis of diabetic retinopathy is typically made through eye examinations and imaging methods. The following methods are commonly used:
- Fundus photography: This involves taking photographs of the retina to visualize damage.
- Optical Coherence Tomography (OCT): This method allows for a detailed view of the eye's internal structure.
- Fluorescein Angiography: This test is used to examine how blood vessels function.
What Are the Treatment Options for Diabetic Retinopathy?
The treatment of diabetic retinopathy can vary depending on the stage and severity of the disease. Treatment options include the following:
- Diabetes control: Maintaining strict control of blood sugar levels helps slow the progression of diabetic retinopathy.
- Laser treatment: This method is used to stop or close leaking blood vessels on the retina.
- Intravitreal injections: Injecting medication into the eye to reduce inflammation in the retina.
- Vitrectomy: A surgical procedure performed to correct bleeding or traction within the eye.
Early diagnosis and treatment of diabetic retinopathy help preserve eye health and prevent vision loss. Therefore, regular eye exams are essential for diabetes patients. Additionally, ensuring diabetes control plays a significant role in reducing the risk of diabetic retinopathy. If you notice symptoms of diabetic retinopathy, it is important to consult your eye doctor immediately. Remember that early diagnosis and treatment prevent vision loss and protect your eye health.

Op. Dr. Şehriyar Hanhüseyinli
Ophthalmologist





