
Keratoconus: A Silent Threat to Our Vision
- Keratoconus: A Silent Threat to Our Vision
- What Is Keratoconus?
- Who Is at Risk?
- What Are the Symptoms?
- How Is It Diagnosed?
- What Are the Treatment Options?
- In Conclusion…
As an ophthalmologist, one of the most frequently encountered corneal diseases in my clinical practice is keratoconus. At first glance, this condition may seem like a simple refractive error such as myopia or astigmatism, but it is in fact a progressive disease that, if left untreated, can lead to permanent vision loss. In this article, I aim to explain—both from a clinical perspective and based on patients’ experiences—what keratoconus is, how it progresses, how it is diagnosed, and what treatment options are available.
What Is Keratoconus?
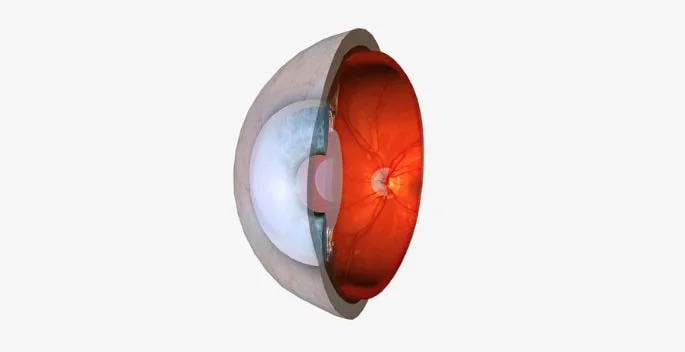
Keratoconus is a degenerative eye condition characterized by the thinning and forward bulging of the cornea—the transparent front layer of the eye—into a cone-like shape. Normally, the cornea has a dome-shaped structure, but in keratoconus, it loses its structural integrity, becomes thinner, irregular, and the quality of vision is significantly reduced.
This distortion prevents light from focusing properly on the retina. As a result, patients usually develop myopia and irregular astigmatism. However, these refractive errors cannot be easily corrected with glasses, as the surface of the cornea is no longer uniformly curved.
Who Is at Risk?
Keratoconus typically begins during adolescence and may progress into the late twenties. It can affect one or both eyes, although one eye is often more severely affected than the other. It occurs in both males and females.
Key risk factors include:
- Genetic predisposition: Those with a family history of keratoconus are at increased risk.
- Chronic eye rubbing: Especially in individuals with allergic eye conditions, habitual eye rubbing may contribute to the development of keratoconus.
- Systemic disorders: Conditions such as Down syndrome and Marfan syndrome (connective tissue disorders) have been associated with keratoconus.
What Are the Symptoms?
Keratoconus usually begins subtly. Patients often report frequent changes in their eyeglass prescription. Over time, the quality of vision continues to decline. Common symptoms include:
- Blurred or distorted vision
- Halos and glare around lights
- Noticeable decline in night vision
- Inadequate vision correction even with glasses
- Eye fatigue and headaches
How Is It Diagnosed?
For diagnosing keratoconus, I utilize advanced imaging techniques. Devices such as corneal topography and tomography allow us to map the surface of the cornea in detail. These tests clearly reveal the thinning, steepening, and irregularity of the cornea.
In some cases, the disease may present no symptoms in its very early stages. That’s why regular eye check-ups are especially important for individuals with a family history of keratoconus.
What Are the Treatment Options?
The goals in treating keratoconus are twofold: to stop the progression of the disease and to restore the best possible visual clarity. The treatment plan is tailored to the stage of the disease:
- Glasses and Soft Contact Lenses: In early stages, if the corneal irregularity is mild, vision may be improved with glasses or soft contact lenses. However, these options often become insufficient as the disease progresses.
- Rigid Gas Permeable Lenses: As corneal irregularity increases, specially designed rigid lenses can help reshape the corneal surface, providing much clearer vision. Though adaptation may be challenging, the improvement in visual quality is substantial.
- Hybrid and Scleral Lenses: For patients who cannot tolerate rigid lenses, hybrid lenses (rigid center, soft periphery) or scleral lenses (large-diameter lenses) offer increased comfort while effectively improving vision.
- Corneal Cross-Linking (CXL): This is the most important method for halting keratoconus progression. By applying riboflavin (vitamin B2) drops and activating them with UV-A light, the collagen fibers within the cornea are bonded together, strengthening the corneal structure. This procedure is most effective when applied in the early stages.
- Intracorneal Ring Segments (ICR): Semi-circular plastic segments are inserted into the cornea to help flatten and reshape it. This can partially restore vision and is often combined with cross-linking for better results.
- Corneal Transplantation (Keratoplasty): In advanced keratoconus cases where other treatments are no longer effective, corneal transplantation may be required. Options include penetrating keratoplasty (full-thickness transplant) or deep anterior lamellar keratoplasty (DALK), which replaces only the front layers of the cornea.
In Conclusion…
Keratoconus is a condition that can significantly impair vision and quality of life if not detected early. Fortunately, with advancements in diagnostic technologies and effective treatment options, disease progression can be stopped and visual function preserved.
Anyone experiencing frequent changes in prescription, blurred vision, or difficulty wearing contact lenses should undergo a thorough eye examination. Remember, early diagnosis is always the most effective treatment.
Do not neglect regular eye check-ups—for a healthy life begins with a clear view.

Dr. Lecturer Konuralp YAKAR
Ophthalmologist




