
Breast Masses and Breast Cancer
- Breast Masses and Breast Cancer
- Goals in Early-Stage Breast Cancer
- Breast Cancer and Surgical Treatment
- Surgical Treatment Options
- What is Breast-Conserving Surgery?
- Sentinel Lymph Node Biopsy
- Goals of Breast-Conserving Therapy (BCT)
- Oncoplastic Breast-Conserving Surgery
- Contraindications for Breast-Conserving Therapy (BCT)
- When to Switch from Breast-Conserving Surgery to Mastectomy?
- Is Recurrence Higher with Breast-Conserving Surgery Compared with Mastectomy?
- Advantages of Breast-Conserving Surgery Over Mastectomy
- Does Cutting the Breast During Breast-Conserving Surgery Exacerbate Breast Cancer?
The risk of breast cancer exists at all ages, but it increases with age. In women aged 20-40, the most common breast mass is fibroadenoma, while in those aged 35-40, breast cysts are the most frequently encountered mass. After the age of 40, the most common breast mass is breast cancer. It is known that one in every eight women will be diagnosed with breast cancer during her lifetime (Figures 1, 2).
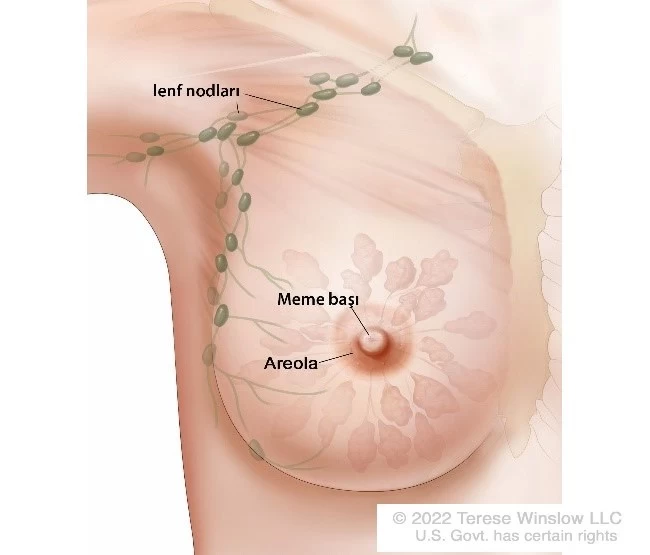
Figure 1: Breast and axillary lymph nodes (Marcus Galea. Benign breast disorders. Surgery (Oxford) 2016;34:19-24)
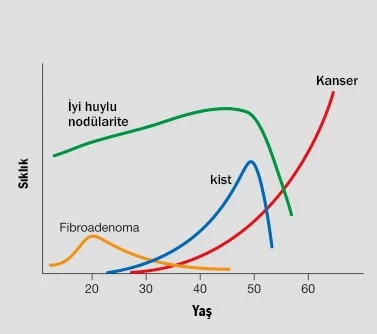
Figure 2: Age Distribution of Breast Masses (Adapted from Marcus Galea. Benign breast disorders. Surgery (Oxford) 2016;34:19-24)
In patients diagnosed with breast cancer, surgery is usually the first treatment option. For early-stage breast cancer, chemotherapy and targeted therapy may also be applied before surgery, depending on the planned type of surgery and the biological characteristics of the tumor.
Goals in Early-Stage Breast Cancer
- Curative Treatment of Breast Cancer
- Low local-regional recurrence
- Disease-free survival (long disease-free survival)
- Survival (long-term survival)
- Achieving Good Cosmesis (aesthetic preservation of the breast)
- Quality of Life (aiming for a high quality of life)
Breast Cancer and Surgical Treatment
Breast cancer is a common disease affecting women of all ages, with forms ranging from very slow-growing to highly aggressive. Understanding the best approach to treat each individual and their cancer is a complex task. Treatment of breast cancer had stunning developments over the years. To date, patients are offered more advanced and less extensive surgical options. Factors such as the patient’s age, tumor size, breast structure and size, tumor’s biological characteristics, status of the axillary lymph nodes, and patient preference influence the choice of surgical procedures for breast cancer.
Surgical Treatment Options
The choice of surgery depends on several factors. The patient and doctor should decide together on the most appropriate surgical approach, considering individual factors such as the stage of breast cancer, tumor and breast size, and age. The doctor and patient should discuss the risks and benefits of breast-conserving surgery versus mastectomy, selecting the option that provides the most comfort and peace of mind for the patient in the long term.
- Mastectomy: The removal of the entire breast tissue, including the nipple, areola (the pigmented area around the nipple), and surrounding breast skin.
- Breast-Conserving Surgery
- Standard breast-conserving surgery (tumor removal without oncoplastic techniques)
- Oncoplastic breast-conserving surgery (complete removal of the tumor while preserving breast aesthetics)
- Bilateral reduction mammoplasty (aesthetic reshaping of the breasts)
- Mastectomy and Breast Reconstruction
- Reconstruction with silicone implants
- Reconstruction using the latissimus dorsi (back muscle) or rectus abdominus muscles (abdominal muscles)
What is Breast-Conserving Surgery?
Breast-conserving surgery is currently the gold standard for early-stage breast cancer and one of the most commonly performed breast procedures. This surgery aims to completely remove the tumor along with a margin of normal breast tissue while ensuring negative surgical margins. It is also known as lumpectomy (removal of the lump), partial (segmental) mastectomy, quadrantectomy (removal of the tumor-containing section of the breast), or breast-conserving surgery (BCS). The primary goals are to minimize the risk of cancer recurrence and maintain breast aesthetics. Breast-conserving surgery (BCS) enables breast conserving without compromising oncologic outcomes.
Sentinel Lymph Node Biopsy
Alongside segmental mastectomy, a sampling biopsy of the axillary (underarm) lymph nodes is also performed in breast-conserving surgery. This procedure, called sentinel lymph node biopsy (SLNB), involves injecting 5 mL of blue dye into the lymphatic Sappey plexus under the nipple and areola before BCS. The dye travels through the breast tissue, reaching the axillary lymph nodes and marking approximately 3-5 nodes. The dyed lymph nodes are potential sites for the spread of breast cancer to the underarm. SLNB preserves the axilla (underarm area), and it is not inaccurate to refer to SLNB as an axilla-preserving surgical procedure. Previously, axillary lymph node dissection was commonly performed to determine if breast cancer had spread to the lymph nodes. Axillary dissection is a more extensive procedure involving the removal of level 1 and 2 lymph nodes and the lymphoareolar region under the arm.
The advantage of SLNB is that it significantly reduces the risks of lymphedema, pain and numbness in the arm, and limited arm and shoulder movement compared with axillary dissection. Due to the side effects associated with axillary dissection, such as arm edema, it has largely been replaced by sentinel lymph node biopsy (SLNB). By removing the enlarged and the stained lymph nodes in the axilla with SLNB, the axilla could be preserved and complications such as arm edema would be largely avoided. (Figure 3).

Figure 3: Sentinel lymph nodes in the axilla after injection of blue dye into the lymphatic network beneath the breast areola
If the tumor is large relative to the breast size, neoadjuvant chemotherapy (chemotherapy given before surgery) may be administered to shrink the tumor initially.
After breast-conserving surgery (BCS) for breast cancer, radiation therapy is typically applied to the breast. The goal of this radiation is to eliminate any microscopic foci in the remaining breast tissue that may not have been detected through physical examination or imaging. The combination of BCS and radiation therapy is known as breast-conserving therapy (BCT).
The combination of BCS and radiotherapy is known as breast-conserving therapy (BCT), which is now considered the gold standard for early-stage breast cancer.
Goals of Breast-Conserving Therapy (BCT)
- Achieve a good breast aesthetic
- Remove the tumor with negative margins
- Minimize local recurrence
Oncoplastic Breast-Conserving Surgery
To prevent potential deformities in the breast shape post-BCS, oncoplastic surgical techniques can be used to reshape the breast and preserve aesthetics. The term "oncoplasty," derived from "onco" (tumor) and "plasty" (shaping), refers to the surgical approach that combines complete tumor removal with breast aesthetic preservation. This technique involves integrating oncologic and plastic surgery methods.
Who Is Eligible for Breast-Conserving Therapy (BCT)?
- Applicable to patients of all ages.
- Suitable for early-stage breast cancer: This includes tumors confined to the breast, without distant metastasis, minimal spread to axillary lymph nodes (spread to fewer than four lymph nodes), and tumors smaller than 5 cm. A larger tumor size is not an absolute contraindication; however, in cases where the breast is small and the tumor is large, achieving. If the breast is large enough to accommodate a tumor greater than 5 cm (a suitable tumor-to-breast ratio), BCT may still be an option. In such cases, oncoplastic techniques can help prevent aesthetic deformities due to the extensive tissue removal (Oncoplastic Breast-Conserving Surgery) (Figures 4 and 5).
- Applicable to patients without contraindications for breast radiotherapy.
- Clear negative surgical margins should be achievable around the tumor and the surrounding healthy tissue.
- For patients with larger tumors where significant deformity is expected, neoadjuvant chemotherapy (NACT) may be administered pre-surgery to reduce tumor size, making BCT feasible if the tumor shrinks or disappears.
- Patients with multicentric tumors (multiple tumors in different quadrants) may also be eligible for BCT if oncoplastic techniques are used to maintain breast aesthetics (Oncoplastic Breast-Conserving Surgery).

Figure 4: Bilateral Oncoplastic Breast-Conserving Surgery Using the Racquet Technique for Bilateral Braest Cancer

Figure 5: Oncoplastic Breast-Conserving Surgery Using the Donut Technique for Right Breast Cancer
Contraindications for Breast-Conserving Therapy (BCT)
Breast-conserving therapy is typically applicable for early-stage breast cancer. However, it is not suitable for locally advanced (Stage 3) or metastatic breast cancer (Stage 4). For locally advanced (T4) tumors—cases in which extensive lymphedema causes the breast to appear like an orange peel, where the tumor is fixed to the chest wall muscles, or where the tumor has invaded the skin causing ulceration—BCT is generally not feasible. In such cases, chemotherapy may be administered first to downstage or shrink the tumor, enabling the possibility of BCT.
For BCT to be performed, postoperative radiotherapy should be able to be given to whole breast. Some conditions, such as active connective tissue diseases (e.g., systemic lupus erythematosus, scleroderma), are relative contraindications for BCT, as radiation may yield suboptimal aesthetic outcomes due to poor skin perfusion. Furthermore, acceptable cosmetic results after BCT are essential, meaning the surgery should leave the breast with a satisfactory appearance. In cases of large tumors relative to breast size, achieving satisfactory breast aesthetics post-surgery could be challenging. For large tumors where breast aesthetics are difficult to maintain, BCT may not be advisable, and oncoplastic BCT may be considered.
The presence of suspicious or malignant appearing microcalcifications that cover the entire breast on mammography is a contraindication to BCT, as they likely indicate extensive cancer across the breast, making breast preservation unsuitable. Diffuse ductal carcinoma in situ (DCIS) and inflammatory breast cancer are also contraindications for BCT. Additionally, if after two BCT attempts the surgical margin remains positive (indicating persistent tumor presence), mastectomy becomes the preferred approach.
Pregnancy is another contraindication for BCT, particularly in the first and second trimesters, as radiation therapy is not appropriate during pregnancy. However, BCT may be feasible in the third trimester (the last three months), as radiation therapy can be administered post-delivery. For patients with genetic mutations such as BRCA1 or BRCA2, BCT is not strictly contraindicated. However, in patients 35 years or younger with a BRCA1 or BRCA2 mutation, BCT is generally discouraged due to a higher risk of recurrence compared with mastectomy.
When to Switch from Breast-Conserving Surgery to Mastectomy?
If after a second BCT attempt the surgical margin remains positive (persistent surgical margin positivity), a switch to mastectomy is recommended.
Is Recurrence Higher with Breast-Conserving Surgery Compared with Mastectomy?
Complete breast removal (mastectomy) does not eliminate the risk of breast cancer recurrence or a new cancer. Randomized studies—the most robust and reliable form of scientific evidence—show that recurrence rates in BCT patients are not significantly higher than in mastectomy patients. These studies also indicate no survival difference between mastectomy and BCT. Among well-selected patients with negative surgical margins, the 10-year recurrence rate is below 10%, comparable to mastectomy. Therefore, the desire to avoid local recurrence (or relapse) should not prompt patients eligible for BCT to choose mastectomy.
Advantages of Breast-Conserving Surgery Over Mastectomy
Breast-conserving surgery (BCS) provides several advantages, particularly in terms of preserving body integrity and enhancing the patient's overall quality of life. Here are the key benefits:
- Psychological Benefits: Preserving the breast helps maintain the patient's body image and self-esteem. Patients who undergo BCS tend to have a more positive perception of their body image compared with those who have a mastectomy. This preservation could lead to improved psychosocial well-being.
- Quality of Life: Studies have demonstrated that patients who undergo successful breast-conserving therapy experience higher quality of life across various domains—physiological, sexual, psychological, and social—when compared with those who have undergone mastectomy.
- Body Integrity: Maintaining the breast contributes to the physical integrity of the body, which can positively affect the patient's emotional and mental health. The psychological impact of preserving the breast can could profound, leading to greater satisfaction with the treatment outcome.
Does Cutting the Breast During Breast-Conserving Surgery Exacerbate Breast Cancer?
During breast-conserving surgery, the knife does not directly contact the cancerous breast tissue. Instead, the surgeon removes a portion of healthy breast tissue surrounding the tumor to ensure complete excision. Because the incision is made through the healthy tissue, the risk of cancer spread due to surgical intervention is mitigated.
There is no evidence to suggest that surgical intervention, such as making an incision or performing a biopsy on the breast, causes to spread breast cancer. In fact, existing studies indicate that cutting into breast tissue does not exacerbate cancer.
Prof. Dr. Bekir Kuru
General Surgeon and Surgical Oncologist



