Colon Cancer: The Perspective of A Surgical Oncology Specialist
- Colon Cancer: The Perspective of A Surgical Oncology Specialist
- What are the Symptoms of Colon Cancer?
- What are the Risk Factors for Colon Cancer?
- How is Colon Cancer Diagnosed?
- What are the Treatment Options for Colon Cancer?
- Rehabilitation and Prognosis in Colon Cancer
- Preventive Measures and Conclusion
What is Colon Cancer?
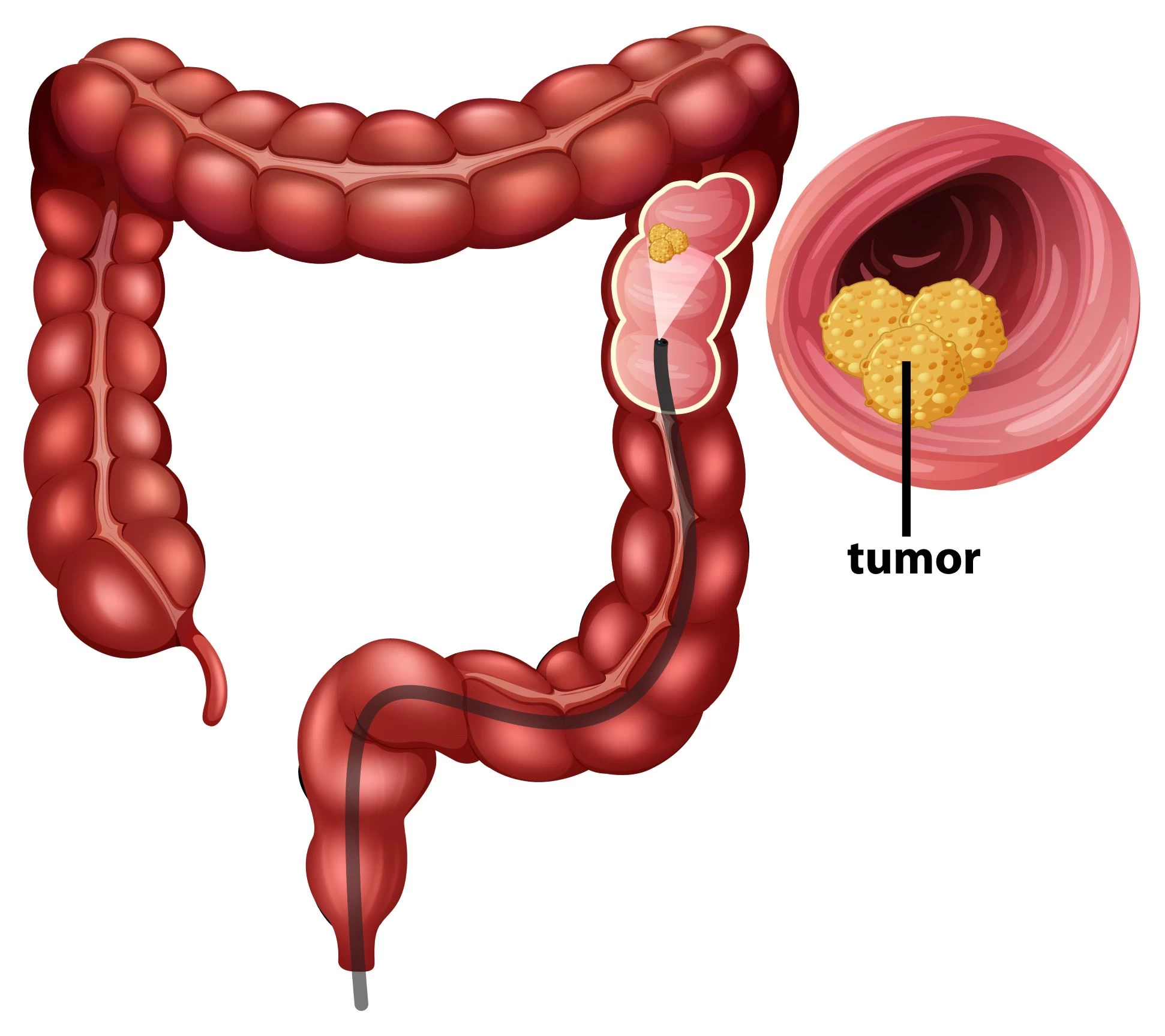
Colon cancer is a type of cancer that begins in the large intestine (colon) or rectum (the area between the anus and the large intestine). Surgical oncology specialists note that colon cancer typically originates from small, initially harmless tumors called polyps. These polyps can transform into cancerous cells over time and, if left untreated, can cause severe health issues in advanced stages.
What are the Symptoms of Colon Cancer?
Colon cancer often does not show symptoms in its early stages. However, as the disease progresses or certain conditions arise, symptoms may appear. The main symptoms of colon cancer are:
- Changes in Bowel Habits: Tumors in the colon affect bowel movements. Persistent diarrhea, constipation, or noticeable changes in bowel habits may be observed.
Bloody Stools or Rectal Bleeding: Colon cancer can damage blood vessels on the inner surface of the rectum or colon, leading to blood in the stool. Seeing blood on toilet paper or in the stool should be taken seriously.
Abdominal Pain or Cramps: Tumors growing inside the intestine can cause pain or cramps in the abdominal area.
Weakness and Fatigue: Cancer consumes the body's energy sources, leading to feelings of weakness and fatigue.
Weight Loss: Loss of appetite and weight loss can be symptoms of colon cancer. The growing tumor and energy consumption by the body lead to weight loss.
Gas and Bloating: Tumors in the colon can cause gas accumulation and bloating.
Tenesmus: Tumors obstructing the colon can make it difficult for stool to pass, causing a feeling of incomplete evacuation.
Anemia: Colon cancer can cause blood loss during bowel movements, leading to conditions like anemia. Symptoms of anemia include paleness, weakness, and shortness of breath.
These symptoms usually appear in advanced stages; therefore, individuals with risk factors are advised to undergo regular medical check-ups and screening tests.
What are the Risk Factors for Colon Cancer?
There are several risk factors for colon cancer. However, having these risk factors does not necessarily mean that a person will develop colon cancer; they only increase the risk. Here are the risk factors for colon cancer:
- Age: Colon cancer generally increases with age and is more common in individuals over 50.
Family History: Individuals with a family history of colon or rectal cancer may be at risk. The risk is higher if a first-degree relative (parents, siblings, children) has had colon cancer.
Personal History: Individuals who have previously had colon cancer or polyps in the intestine are at risk of developing the disease again.
Inflammatory Bowel Diseases: Chronic inflammatory bowel diseases, particularly long-term ulcerative colitis or Crohn's disease, increase the risk of colon cancer.
Genetic Syndromes: Hereditary genetic syndromes can increase the risk of colon cancer. Examples include Lynch syndrome and FAP (Familial Adenomatous Polyposis), which are associated with genetic mutations.
History of Polyps: Especially adenomatous polyps can increase the risk of colon cancer as these types of polyps often become cancerous.
Other Cancers: Individuals who have had other cancers such as liver, uterus, or ovarian cancer may have an increased risk of colon cancer.
Diet: Diets high in fat and low in fiber can increase the risk of colon cancer. It is also associated with excessive consumption of red and processed meats.
Smoking and Alcohol Use: Smoking and excessive alcohol consumption can increase the risk of colon cancer.
Obesity: Being overweight or obese can increase the risk of colon cancer.
Lack of Physical Activity: Not exercising regularly can increase the risk of colon cancer.
These risk factors can vary depending on an individual’s overall health, genetic traits, and lifestyle. Individuals with these risk factors are advised to have regular medical check-ups and recommended screening tests to improve the chances of early diagnosis and treatment of colon cancer.
How is Colon Cancer Diagnosed?
Several medical tests and methods are used for the accurate diagnosis of colon cancer. The diagnostic process generally involves several steps, determined based on the patient's symptoms, risk factors, and medical history. Here are the main methods used to diagnose colon cancer:
- Physical Examination and Medical History: We take a detailed medical history of the patient's general health, symptoms, and family history. We also examine the abdominal area to evaluate for signs such as tumors or masses.
Laboratory Tests: Blood tests are used to detect anemia (low blood count) or other symptoms associated with colon cancer. We also check for specific tumor markers like CEA (carcinoembryonic antigen).
Imaging Tests:
- Colonoscopy: One of the most trusted diagnostic methods for colon cancer. A flexible tube with a camera is used to visualize the inside of the intestine and detect tumors and polyps.
- Sigmoidoscopy: Similar to colonoscopy but uses a shorter tube. It is generally used to examine the lower parts of the intestine.
- Barium Enema: Barium coats the intestines, providing better contrast on X-ray images, which helps in detecting tumors and changes in the intestine's inner surface.
- Computed Tomography (CT) or Magnetic Resonance Imaging (MRI): These imaging techniques are used to evaluate the size, spread, and impact of tumors on surrounding tissues.
Biopsy: During a colonoscopy or other imaging tests, we take small samples from abnormal-looking tissues. These samples are sent to the pathology lab, where they are examined by pathologists. If cancer cells are present, a diagnosis is made.
Genetic Tests: In some cases, based on family history, genetic tests may be conducted, particularly for individuals at risk of hereditary cancer syndromes.
What are the Treatment Options for Colon Cancer?
The treatment of colon cancer is determined based on the patient's overall health, the stage and type of cancer, and other individual factors. A multidisciplinary approach usually provides the most effective results, and treatment typically involves a combination of surgery, chemotherapy, radiation therapy, and targeted therapies. Here is an overview of the treatment options for colon cancer:
- Surgical Intervention:
- Colon Resection: A surgical procedure to remove the cancerous section of the intestine. The healthy ends of the intestine are then joined.
- Laparoscopic Surgery: A surgical method using small incisions. It is less invasive and speeds up the recovery process.
Chemotherapy: Chemotherapy involves the use of drugs to kill cancer cells or prevent them from multiplying. In colon cancer, it is used before or after surgery, in cases of metastasis, or when cancer is incurable.
Radiotherapy: Radiotherapy uses high-energy rays to kill cancer cells. It is used before or after surgery to shrink tumors or control cancer cells that have spread to surrounding tissues.
Targeted Therapies: Targeted drugs focus on cells with specific genetic or biochemical properties. This therapy is often used in combination with chemotherapy or as an alternative.
Immunotherapy: Immunotherapy strengthens the immune system or targets cancer cells. While not widely used yet in colon cancer treatment, research is ongoing.
Perfusion Therapies: In some cases, special treatments like isolated liver perfusion are considered for patients with liver metastases.
The treatment plan is personalized based on the patient’s overall health, the stage of cancer, and other individual factors. The success of treatment depends on the patient's response and the stage of cancer.
Rehabilitation and Prognosis in Colon Cancer
After surgical intervention, as surgical oncology specialists, we support the rehabilitation process and provide recommendations to improve the quality of life for our patients. Prognosis varies depending on the stage of the disease, response to treatment, and other factors. Many patients successfully overcome colon cancer with early diagnosis and a comprehensive treatment plan.
Preventive Measures and Conclusion
As surgical oncology specialists, we emphasize that a healthy lifestyle can reduce the risk of colon cancer. Regular exercise, a balanced diet, a low-fat diet, and regular screening tests help prevent colon cancer. In conclusion, the treatment of colon cancer requires a multidisciplinary approach. Surgical oncology specialists play a critical role in creating personalized treatment plans tailored to the individual needs of patients. Throughout this process, patients should closely cooperate with surgical oncology specialists, prioritize regular follow-up and screenings, and maintain a healthy lifestyle.
Stay healthy…

Assoc. Prof. Dr. Oktay Karaköse
General Surgery and Surgical Oncology Specialist