
Targeted Therapy and Immunotherapy in Cancer
- Targeted Therapy and Immunotherapy in Cancer
- Targeted Therapy
- Which Cancer Types Respond to Targeted Therapy?
- Immunotherapy Drugs
- Immunotherapy in Combination Treatments
Cancer remains one of the most significant health problems today. Fundamentally, this disease is characterized by the uncontrolled proliferation of cells and can originate from almost any cell type. For many years, conventional treatment methods such as surgery, radiotherapy, and chemotherapy have been utilized, and they still constitute the main components of cancer treatment today.
Targeted Therapy
However, since the early 2000s, a new era has begun in cancer treatment with the introduction of what is known as “targeted therapies.” Commonly referred to as “smart drugs” by the public, these treatments work by targeting the mechanisms responsible for the growth and proliferation of cancer cells. These drugs affect the systems that transmit signals from specific receptors on the cell surface to the nucleus via various intracellular biological pathways. By blocking these surface receptors or intracellular signaling pathways at different levels, they prevent the uncontrolled proliferation of cancer cells. Among these drugs are monoclonal antibodies, tyrosine kinase inhibitors, angiogenesis inhibitors, EGFR inhibitors, proteasome inhibitors, and mTOR inhibitors.
Which Cancer Types Respond to Targeted Therapy?
Targeted therapies can yield highly effective results, especially when used alone or in combination with chemotherapy in certain cancer types. However, these therapies are not suitable for all cancer patients; they are used only in cases with specific diagnoses and where certain biological markers have been identified. The cancers in which targeted therapies are most effective include breast cancer, non-small cell lung cancer, chronic myeloid leukemia, colorectal cancer, malignant melanoma, renal cell carcinoma, gastrointestinal stromal tumors, and ovarian cancer.

Immunotherapy Drugs
Since the early 2010s, developments in immunotherapy—particularly the introduction of immune checkpoint inhibitors (PD-1, PD-L1, and CTLA-4 inhibitors)—have begun to play a role in cancer treatment. These treatments, also commonly referred to as “smart drugs” by the public, work by reactivating the immune system, which has been suppressed by tumor cells. For their pioneering work in this field, Tasuku Honjo and James Allison were awarded the 2018 Nobel Prize in Physiology or Medicine.
Immunotherapy drugs are classified into several main groups. Among the most widely used are PD-1 inhibitors (Nivolumab, Pembrolizumab), PD-L1 inhibitors (Atezolizumab, Durvalumab), and newer agents such as LAG-3 inhibitors (Relatlimab). These drugs enhance the immune system’s ability to recognize and destroy tumor cells. Immunotherapy has shown highly effective results in certain cancer types. The cancers in which immunotherapy is most effective include melanoma, non-small cell lung cancer, renal cell carcinoma, Hodgkin lymphoma, bladder cancer, head and neck cancers, and hepatocellular carcinoma (liver cancer).
Immunotherapy in Combination Treatments
In recent years, these treatment approaches have been studied across almost all types of cancer, and in many cases, they have provided longer progression-free survival and overall survival compared to conventional chemotherapy. The next phase of clinical research has focused on applying immunotherapies in combination with chemotherapy and targeted therapies. These combination strategies have further improved treatment outcomes in many types of cancer and continue to be actively studied.
Since these therapies target more specific mechanisms compared to classical chemotherapy, they generally provide more effective results with fewer side effects. Targeted therapies and immunotherapies represent groundbreaking advances in modern oncology and have secured an important place in the fight against cancer.
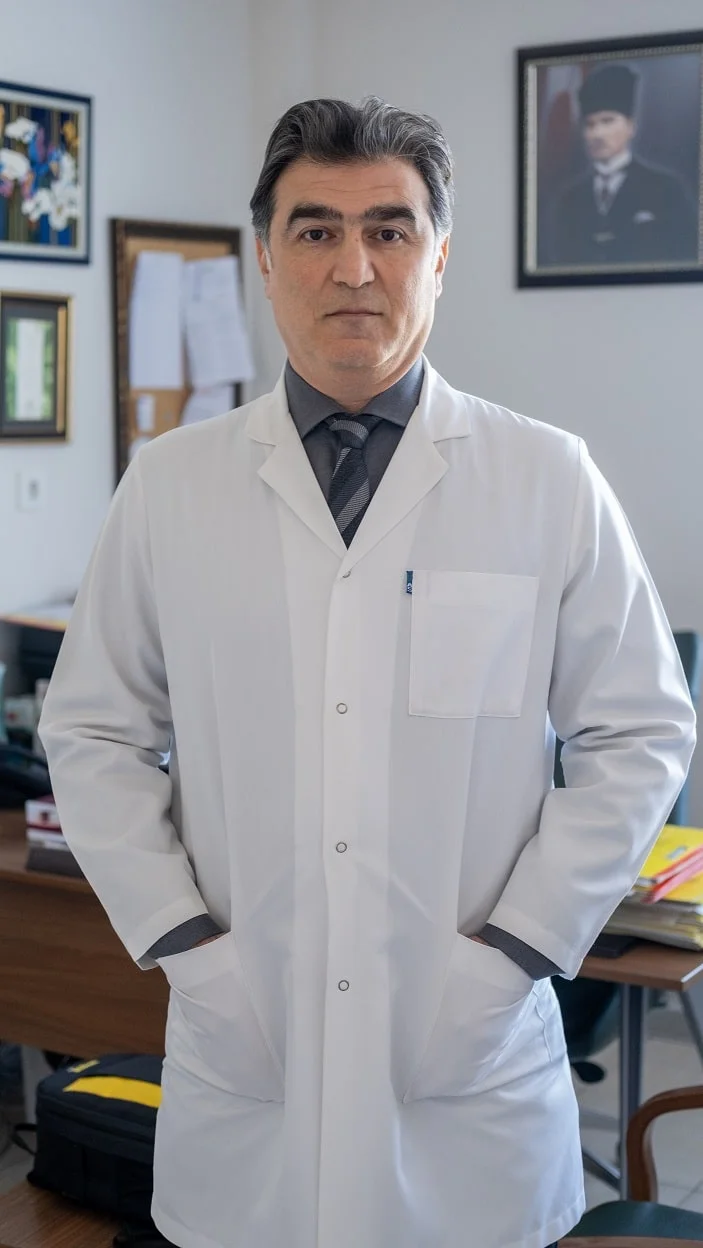
Prof. Dr. Bahiddin Yılmaz
Medical Oncology and Internal Medicine Specialist

