Approach to Chronic Headaches
- Approach to Chronic Headaches
- What Is a Chronic Headache?
- Causes of Chronic Headaches
- Diagnostic Process
- Treatment Approaches
- Patient Education and Follow-Up
- Conclusion
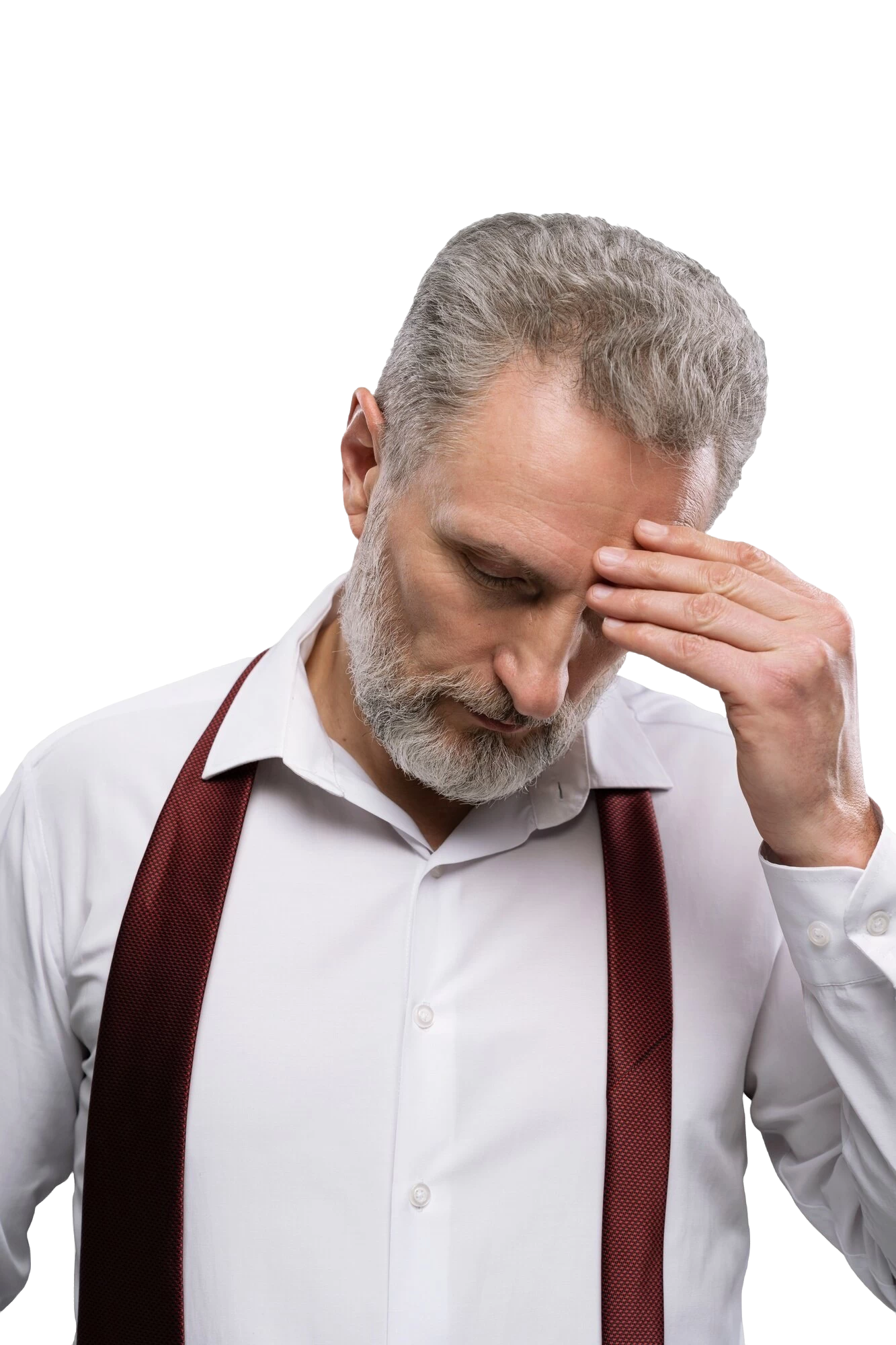
As a pain specialist, chronic headaches are a complex condition that significantly reduce the quality of daily life and negatively affect an individual’s functionality. In this article, I aim to provide detailed information about the definition, causes, classification, and treatment approaches of chronic headaches.
What Is a Chronic Headache?
Chronic headache is defined as a headache that occurs on 15 or more days per month and lasts for more than three months. This condition can be caused by primary or secondary factors. While primary headaches such as migraines or tension-type headaches may become chronic, secondary headaches can arise from causes such as trauma, infections, or tumors.
Causes of Chronic Headaches
The causes of chronic headaches can be diverse and can be grouped as follows:
Primary Headaches:
- Chronic Migraine: Can occur with or without aura and is associated with changes in brain chemicals and genetic predisposition.
- Chronic Tension-Type Headache: Often develops due to stress, anxiety, or muscle tension.
- Cluster Headaches: Characterized by severe pain attacks around the eye, which may sometimes become chronic.
Secondary Headaches:
- Trauma: Post-traumatic headaches following head injuries.
- Infections: Conditions such as sinusitis or meningitis.
- Vascular Causes: Problems in the brain's blood vessels (e.g., aneurysms or arterial dissection).
- Structural Abnormalities: Tumors, increased or decreased intracranial pressure.
Other Factors:
- Sleep disorders.
- Chronic stress or depression.
- Overuse of painkillers (medication-overuse headaches).
Diagnostic Process
The evaluation of chronic headaches involves taking a detailed medical history and performing a thorough physical examination. If necessary, advanced diagnostic tools may be employed, such as:
- Imaging Techniques: Magnetic Resonance Imaging (MRI) or Computed Tomography (CT) to rule out structural causes.
- Blood Tests: If an infection or systemic disease is suspected.
- Eye Examination: To detect conditions such as optic nerve compression.
- Sleep Studies: To assess for sleep apnea or other sleep disorders.
Treatment Approaches
Managing chronic headaches requires a multidisciplinary approach tailored to the underlying cause and the individual needs of the patient.
Pharmacological Treatments:
- Prophylactic Medications: Beta-blockers, antidepressants, or antiepileptic drugs for conditions like migraines.
- Acute Treatments: Triptans or nonsteroidal anti-inflammatory drugs (NSAIDs).
- Prevention of Medication Overuse: Patient education to avoid excessive use of painkillers.
Non-Pharmacological Methods:
- Cognitive Behavioral Therapy (CBT): Effective for stress management and relaxation techniques.
- Physical Therapy and Rehabilitation: Exercises to relax neck and shoulder muscles.
- Dietary Modifications: Identifying and avoiding migraine triggers (e.g., caffeine, chocolate).
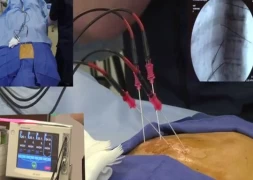
Interventional Methods:
- Nerve Blocks: Occipital nerve block can be effective in chronic headaches.
- Botulinum Toxin Injections: FDA-approved for chronic migraine treatment.
- Neuromodulation: Techniques such as vagus nerve or occipital nerve stimulation.
Complementary and Alternative Medicine:
- Acupuncture.
- Ozone therapy.
- Meditation and yoga.
Patient Education and Follow-Up
The success of headache treatment depends not only on the treatments applied but also on the patient’s adherence to lifestyle changes. Patients should be educated about:
- The importance of maintaining regular sleep habits.
- Strategies for stress management.
- Avoiding headache triggers.
- Proper and regular use of medications.
During follow-up, the patient’s response to treatment should be carefully monitored, and the treatment plan should be adjusted as needed.
Conclusion
Chronic headaches can significantly impact an individual’s quality of life. However, with the right approach and personalized treatment, this condition can be effectively managed. As a pain specialist, my priority is to improve my patients' quality of life and help them overcome this challenging condition. Multidisciplinary collaboration, patient education, and continuous follow-up are the most critical elements of treatment success.
It should always be remembered that every patient is unique, and the treatment process must be tailored accordingly.

Assoc. Prof. Dr. Tülin Arıcı
Pain (Algology) Specialist