Shingles Pain: Causes, Symptoms, and Treatment Methods
- Shingles Pain: Causes, Symptoms, and Treatment Methods
- What is Shingles?
- How Does Shingles Pain Develop?
- Symptoms of Shingles Pain
- Treatment of Shingles Pain
- Postherpetic Neuralgia and Long-Term Treatment
- Conclusion
Shingles, medically known as herpes zoster, is an infectious disease that affects nerve tissues and often presents with severe pain. Many of my patients frequently complain about these pains, which can sometimes significantly reduce their quality of life. As a Pain Management Specialist (Algologist), I would like to discuss the development, nature, and treatment methods of shingles pain.
What is Shingles?
Shingles occurs when the chickenpox virus (varicella-zoster), which remains dormant in the body after a childhood infection, reactivates years later when the immune system weakens. This virus hides in the nerve roots and, when reactivated, spreads along the nerves to the skin, causing a rash. However, one of its most important features is the intense pain it causes due to the damage to the nerve tissue.
How Does Shingles Pain Develop?
Shingles pain begins when the virus infects nerve cells. The infected nerve cells can no longer function properly, leading to severe pain in the area served by that nerve. The pain usually starts before the rash appears and can last for weeks, even months, after the rash has healed. This long-lasting pain is called postherpetic neuralgia, which is one of the most common complications of a shingles infection.
My patients often describe shingles pain as a burning, stabbing, sharp, or throbbing sensation. Additionally, sensitivity to touch and electric-like sensations are common in the affected area. This pain, which can disrupt sleep and daily activities, is nerve-related, so traditional painkillers may not always be effective.
Symptoms of Shingles Pain
Shingles pain typically occurs on one side of the body along the distribution of a specific nerve. Symptoms may include:
- Severe pain: Often begins a few days before the rash appears.
- Rash and blisters: After the pain, red patches and fluid-filled blisters develop on the skin.
- Itching and sensitivity: The skin in the affected area becomes sensitive, and even the slightest touch can cause intense pain.
- Burning sensation: Inflammation of the nerves can cause a deep burning feeling.
- Long-term pain due to nerve damage: If postherpetic neuralgia develops, nerve pain can persist for months after the rash has healed.
Postherpetic neuralgia is especially common in elderly patients and is one of the most distressing complications of shingles. It leads to chronic pain in the areas where the nerves have been damaged.

Treatment of Shingles Pain
The primary goal in treating shingles pain is to control the pain as quickly and effectively as possible and prevent the development of postherpetic neuralgia. As a Pain Management Specialist, I develop individualized approaches to manage shingles pain by combining various treatment methods. These treatment options include:
- Antiviral Therapy: Antiviral medications are used to stop the replication of the shingles virus. Drugs like acyclovir and valacyclovir prevent the spread of the rash and reduce the severity of the pain. Early treatment shortens the duration of the infection and reduces the risk of postherpetic neuralgia.
- Pain Relievers: Shingles pain can be extremely intense, and traditional pain relievers may be insufficient. First-line painkillers, such as NSAIDs (nonsteroidal anti-inflammatory drugs), can be used as initial treatment. However, if these are not enough, stronger painkillers or opioids may be required.
- Neuropathic Pain Medications: Since shingles pain is caused by nerve damage, neuropathic pain relievers may be necessary. Medications such as gabapentin and pregabalin help alleviate nerve-related pain by suppressing excessive nerve activity, thereby improving patients' quality of life.
- Topical Treatments: Topical creams can also be used for pain control. Lidocaine-containing creams can reduce localized pain, while capsaicin creams may be effective for postherpetic neuralgia. However, capsaicin creams may increase the burning sensation in some patients, so they should be used cautiously.
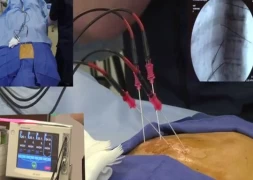
- Nerve Blocks: For patients experiencing severe shingles pain, nerve blocks can be an effective method. Injections made into the nerve root can temporarily block pain signals. These blocks provide significant relief, especially for patients with postherpetic neuralgia.
- Transcutaneous Electrical Nerve Stimulation (TENS): TENS devices, which stimulate nerves through electrodes placed on the skin, can help relieve pain. This method can be an additional treatment option, especially for managing neuropathic pain.
- Psychological Support and Rehabilitation: Chronic pain can also have a negative psychological impact on individuals. In patients with postherpetic neuralgia, emotional issues such as depression and anxiety may arise. Psychological support can help improve quality of life and the treatment process in pain management.
Postherpetic Neuralgia and Long-Term Treatment
Postherpetic neuralgia is the nerve pain that continues after the shingles rash has healed, and it is particularly common in elderly individuals. This type of pain can last for months, even years. If left untreated, it can severely impact a patient's daily life. Neuropathic pain medications, nerve blocks, and TENS play an important role in the treatment of postherpetic neuralgia. A multidisciplinary approach is essential to prevent the chronicity of the pain and to provide long-term relief.
Conclusion
Shingles pain is a severe pain that can significantly reduce quality of life and affects the nerves. The primary goal in treatment is to control the pain quickly and prevent complications such as postherpetic neuralgia. As pain specialists, we aim to maintain both the physical and psychological well-being of patients with a multidisciplinary approach. Tailoring treatment plans according to each patient’s individual needs is key to relieving pain and improving their quality of life.

Assoc. Prof. Dr. Tülin Arıcı
Pain Management Specialist