What is Fatty Liver?
- What is Fatty Liver?
- What are the Symptoms of Fatty Liver?
- Who Can Have Fatty Liver?
- What Should Be Done for Fatty Liver?
- What Should Not Be Done for Fatty Liver?
- How is Fatty Liver Treated?
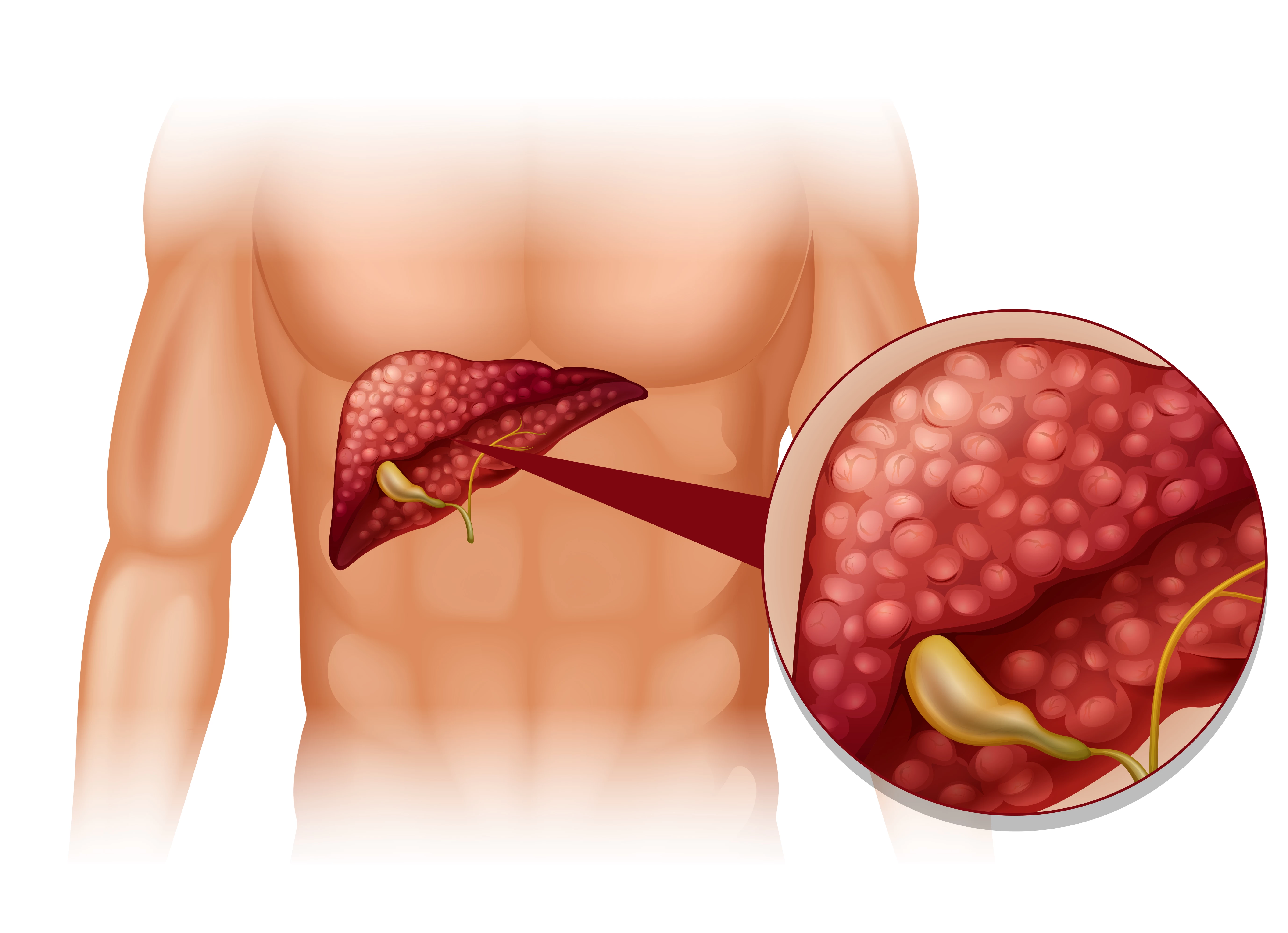
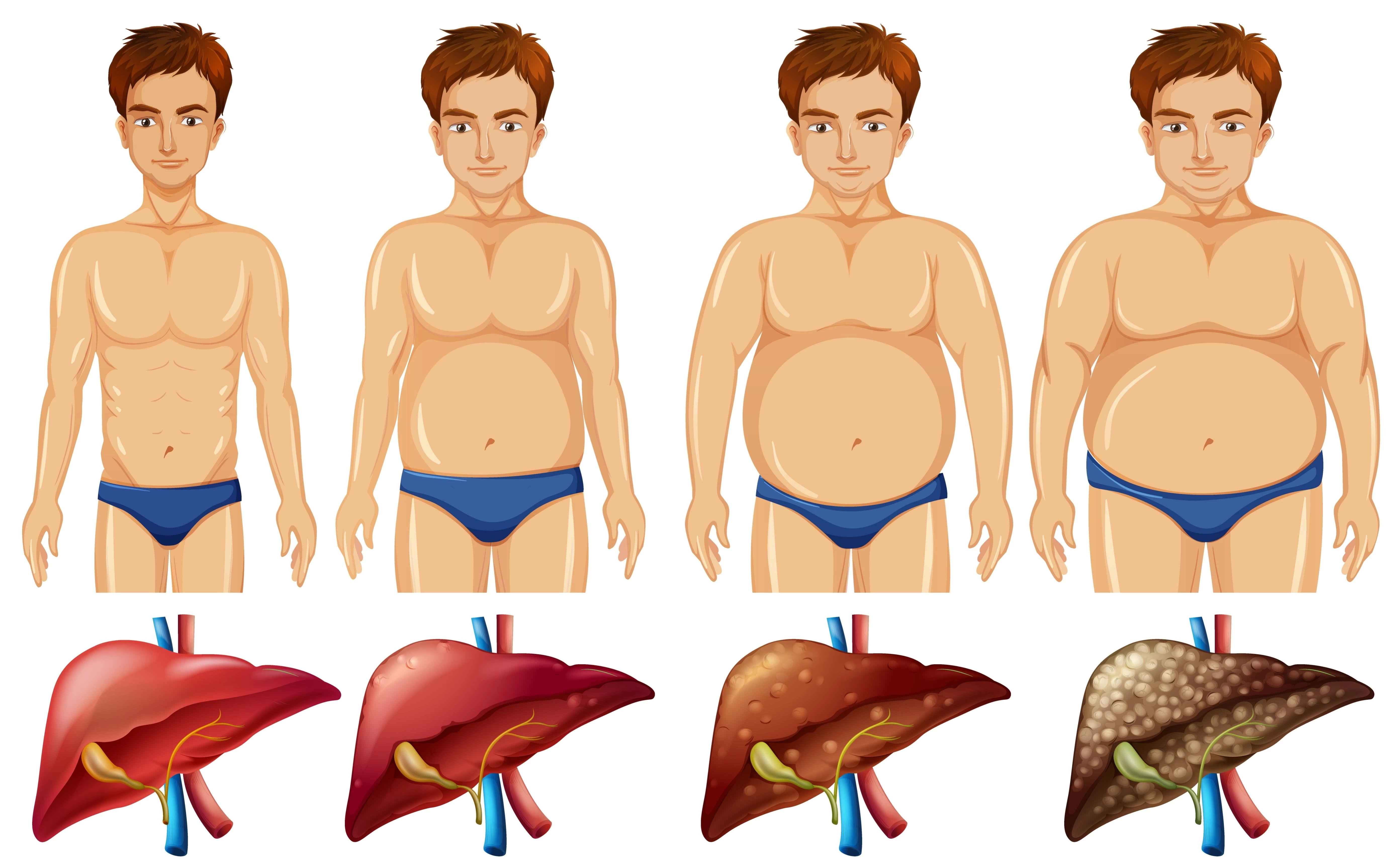
Fatty liver, also known as hepatic steatosis, is a condition characterized by the accumulation of fat in liver cells. It is a common liver disease that can occur for a variety of reasons. Excess fat accumulation in the liver can disrupt its normal function and lead to inflammation, scarring and potential liver damage if left untreated.
There are two main types of fatty liver:
- Non-Alcoholic Fatty Liver Disease (NAFLD): This is seen in individuals who do not consume excessive alcohol. It is often associated with obesity, insulin resistance, diabetes, high blood pressure, and high cholesterol levels. NAFLD is considered a spectrum of conditions ranging from simple fatty liver (steatosis) to nonalcoholic steatohepatitis (NASH), which includes inflammation and liver cell damage.
- Alcoholic Fatty Liver Disease: As the name suggests, this condition is caused by excessive alcohol consumption. Alcohol is processed in the liver and heavy or prolonged drinking can cause fatty buildup in liver cells, leading to Fatty Liver Alcoholic Disease. Over time, if alcohol consumption continues, it can progress to more serious forms of liver damage, such as alcoholic hepatitis and cirrhosis.
The symptoms of fatty liver may disappear or be nonspecific, especially in the early stages. However, as the condition progresses, individuals may experience fatigue, abdominal discomfort or pain, weakness and weight loss. Complications such as liver cirrhosis, liver failure and liver cancer may develop in advanced stages.
Diagnosis of fatty liver typically includes a combination of medical history evaluation, physical examination, blood tests to assess liver function, imaging studies (such as ultrasound, computed tomography, or magnetic resonance imaging), and sometimes a liver biopsy to determine the extent of liver damage.
Fatty liver treatment focuses on addressing underlying causes and making lifestyle changes. This includes following a healthy diet, losing weight if overweight or obese, exercising regularly, managing diabetes, controlling cholesterol levels, avoiding or reducing alcohol consumption, and following prescription medications or interventions recommended by a specialist physician.
If you suspect you have fatty liver or liver-related concerns, it's important to consult a healthcare professional for proper diagnosis, evaluation, and guidance.
What are the Symptoms of Fatty Liver?
Fatty liver, also known as hepatic steatosis, is a condition characterized by the accumulation of fat in liver cells. It can be divided into two types: Alcoholic Fatty Liver Disease (AFLD) and Non-Alcoholic Fatty Liver Disease (NAFLD). The symptoms of fatty liver can vary, and in most cases, the condition may not cause any noticeable symptoms.
However, some common signs and symptoms associated with fatty liver include:
- Fatigue: General fatigue and weakness may occur due to liver inflammation and liver dysfunction.
- Abdominal discomfort: Some people may experience a dull or aching pain in the upper right side of the abdomen. This may be accompanied by a feeling of fullness or bloating.
- Weight loss or loss of appetite: In some cases, people with fatty liver may experience decreased appetite or unintentional weight loss.
- Weakness and confusion: As the condition progresses, there may be neurological symptoms such as difficulty concentrating, memory problems and confusion.
- Enlarged liver: In more advanced cases, the liver may enlarge, causing a feeling of tenderness or heaviness in the right upper abdomen.
- Jaundice: Although less common, severe fatty liver disease can lead to jaundice, which is characterized by yellowing of the skin and eyes.
- Spider veins and easy bruising: The liver is involved in blood clotting, so liver dysfunction can lead to increased skin bruising and the development of spider veins.
It is important to note that these symptoms may also be associated with other liver conditions or health problems. An accurate diagnosis can be made by a healthcare professional through a combination of medical history, physical examination, blood tests, imaging studies (such as an ultrasound or CT scan), and sometimes a liver biopsy.
If you suspect you may have fatty liver or are experiencing any related symptoms, it is recommended that you consult a healthcare professional for proper diagnosis and appropriate management.
Who Can Have Fatty Liver?
Fatty liver disease, also known as hepatic steatosis, can affect a wide variety of individuals. There are two main types of fatty liver disease: alcoholic fatty liver disease (AFLD) and nonalcoholic fatty liver disease (NAFLD).
- Alcoholic Fatty Liver Disease (AFLD): AFLD is caused by excessive alcohol consumption. People who regularly drink large amounts of alcohol are at risk. This condition can progress from simple fatty liver to alcoholic hepatitis and eventually cirrhosis if alcohol consumption continues.
- Non-Alcoholic Fatty Liver Disease (NAFLD): NAFLD is characterized by excessive accumulation of fat in the liver in individuals who consume little or no alcohol.
The following factors increase the risk of developing NAFLD:
- Obesity: People who are overweight or obese, especially those with central obesity (excess belly fat), are more prone to NAFLD.
- Type 2 Diabetes: Individuals with type 2 diabetes have a higher risk of developing NAFLD.
- Insulin Resistance: Insulin resistance, a condition in which body cells do not respond properly to insulin, is strongly associated with NAFLD.
- Metabolic Syndrome: This includes a range of conditions such as high blood pressure, high blood sugar, excess body fat around the waist, and abnormal cholesterol levels.
- Sedentary Lifestyle: Lack of physical activity or a sedentary lifestyle can contribute to the development of NAFLD.
- Unhealthy Diet: Processed foods, sugary drinks, and a diet high in saturated fat can increase the risk.
- Certain Medical Conditions: Certain medical conditions, such as polycystic ovary syndrome (PCOS) and sleep apnea, are linked to an increased risk of NAFLD.
- Medications: Some medications such as corticosteroids, tamoxifen and antiretroviral drugs used in HIV treatment can contribute to the development of fatty liver.
It is important to remember that fatty liver disease can also occur in people who do not have any of the above risk factors. If you suspect you have fatty liver disease or are concerned about your liver health, it is best to consult a healthcare professional for proper diagnosis and appropriate guidance.
What Should Be Done for Fatty Liver?
Fatty liver, also known as hepatic steatosis, is a condition characterized by the accumulation of fat in liver cells. It can be caused by a variety of factors, including obesity, diabetes, high cholesterol, excessive alcohol consumption, and certain medications.
If you have been diagnosed with fatty liver disease, here are some steps you can take to manage and improve the condition:
- Lifestyle changes: Adopting a healthy lifestyle is very important for managing fatty liver. Focus on maintaining a balanced diet rich in fruits, vegetables, whole grains, lean proteins and healthy fats. Limit your intake of processed foods, saturated fats, and added sugar. Also, try to do regular physical activity as it can help reduce liver fat.
- Weight loss: If you are overweight or obese, it is often recommended to lose weight to improve fatty liver. Gradual and steady weight loss through a combination of diet and exercise can help reduce liver fat and improve liver health. However, crash diets or rapid weight loss can be harmful, so it's important to consult a healthcare professional or registered dietitian for guidance.
- Manage underlying conditions: If you have diabetes, high cholesterol, or other underlying conditions that contribute to fatty liver, it is important to manage them effectively. Work with your healthcare provider to develop a treatment plan that includes medications, lifestyle changes, and regular monitoring.
- Limit alcohol consumption: Excessive alcohol consumption can worsen fatty liver and lead to more serious liver disease. If you have fatty liver, it's important to avoid alcohol completely or limit your intake according to your healthcare provider's recommendations.
- Avoid hepatotoxic substances: Some drugs, herbal supplements and chemicals can be harmful to the liver. Check with your doctor or pharmacist to make sure any medications or supplements you're taking are not contributing to liver damage.
- Regular medical checkups: It is important to have regular follow-ups with your healthcare provider to monitor your liver health. They may perform blood tests, imaging studies, and other diagnostic tests to evaluate fatty liver progression and related complications.
Remember, fatty liver management should be individualized based on individual circumstances and medical advice. It is important to consult a healthcare professional who can make specific recommendations and monitor your progress.
What Should Not Be Done for Fatty Liver?
When dealing with fatty liver, there are a few things to avoid to improve liver health and prevent further damage.
Here are some things you should not do for fatty liver:
- Excessive alcohol consumption: Alcohol is a major contributor to fatty liver disease. If you have fatty liver, it is very important to avoid or limit alcohol consumption. Even small amounts of alcohol can worsen the condition and lead to more serious liver damage.
- Neglecting a healthy diet: A diet rich in saturated fats, refined carbohydrates and added sugars can worsen fatty liver disease. It is important to avoid processed foods, fried foods, sugary drinks and high-fat dairy products. Instead, focus on a balanced diet rich in fruits, vegetables, whole grains, lean proteins and healthy fats.
- Overeating or gaining excess weight: Fatty liver is closely linked to obesity and excess weight gain. It is important to maintain a healthy weight with regular exercise and portion control. Losing weight gradually under medical supervision can help cure fatty liver disease.
- Ignoring underlying medical conditions: Certain medical conditions such as diabetes, high cholesterol, and high blood pressure can contribute to fatty liver disease. It is important to effectively manage these conditions through appropriate medications, lifestyle changes, and regular medical checkups.
- Self-medicating or taking over-the-counter supplements: Avoid self-medicating or taking over-the-counter supplements without consulting a healthcare professional. Some medications and supplements can have adverse effects on the liver, especially if you already have fatty liver disease. Always seek medical advice before starting any new medication or supplement.
- Neglecting regular exercise: Regular physical activity is beneficial for liver health. Exercise aids weight management, improves insulin sensitivity, and reduces inflammation, all crucial to managing fatty liver disease. Engage in aerobic exercise such as brisk walking, cycling or swimming for at least 150 minutes per week as recommended by health authorities.
- Ignoring medical advice and follow-up appointments: If you have been diagnosed with fatty liver disease, it is important to follow your healthcare provider's advice and attend scheduled appointments. Regular monitoring of liver function tests and imaging studies can help assess disease progression and guide appropriate interventions.
Remember, these guidelines are general recommendations and it is very important to consult a healthcare professional for personalized advice based on your specific situation.
How is Fatty Liver Treated?
Fatty liver disease, also known as hepatic steatosis, refers to the accumulation of fat in the liver. Treatment for fatty liver depends on the underlying cause and the severity of the condition.
Here are some common approaches to treating fatty liver:
- Lifestyle changes: The first line of treatment for fatty liver includes lifestyle changes that can help improve liver health. These changes include:
- Weight loss: If you are overweight or obese, it is usually recommended to lose weight gradually. Even a modest 5-10% weight loss can significantly reduce liver fat. It should not be forgotten that if the rate of weight loss is high, the fat in the liver will increase rather than decrease.
- Healthy eating: Eating a balanced diet low in saturated fats, cholesterol, and refined carbohydrates can help manage fatty liver disease. Focus on consuming fruits, vegetables, whole grains, lean proteins and healthy fats.
- Regular exercise: Doing regular physical activity can help reduce liver fat and improve overall health. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week.
- Avoid alcohol: If alcohol consumption contributes to fatty liver, it is important to avoid alcohol altogether.
- Medications: In some cases, your doctor may prescribe medications to manage certain underlying conditions or to help improve liver health. For example, if you have nonalcoholic fatty liver disease (NAFLD) and associated conditions such as obesity, diabetes, or high cholesterol, you may be given medications to manage these conditions.
- Management of underlying conditions: If fatty liver is caused by an underlying medical condition such as diabetes or high triglycerides, it is very important to treat and manage this condition. Controlling blood sugar levels, managing lipid levels, and addressing other contributing factors are essential to improving liver health.
- Close monitoring and follow-up: Regular monitoring of liver function through blood tests and imaging studies can help monitor disease progression and evaluate the effectiveness of treatment. Your doctor may recommend follow-up visits to assess your condition and make any necessary adjustments to your treatment plan.
It is important to remember that these treatment approaches are general guidelines and the specific treatment plan may vary depending on individual circumstances. If you have been diagnosed with fatty liver disease, it is best to consult a specialist physician who can provide personalized advice and treatment options based on your unique situation.